Osteoporosis
Understanding Osteoporosis
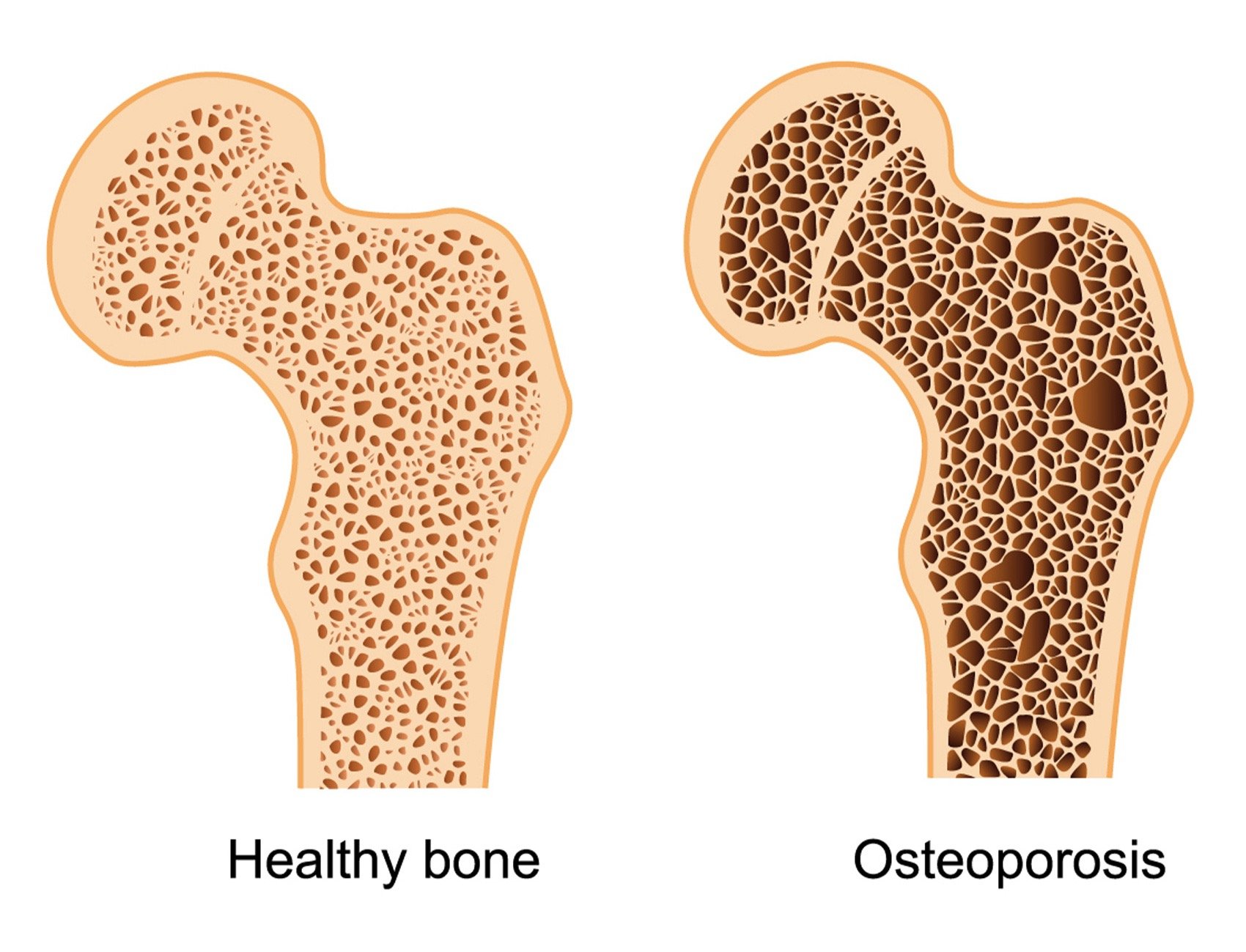
Osteoporosis is a common condition that weakens bones, making them more fragile and prone to fractures. Often called the 'silent disease,' it progresses without noticeable symptoms until a fracture occurs. Maintaining strong bones is essential for overall health, mobility, and independence.
In this guide, we explore the key risk factors for osteoporosis, how to prevent bone loss, and the steps you can take to protect your bone health.
Understanding Osteoporosis: Common Risk Factors
Osteoporosis is a condition that weakens bones, making them more fragile and prone to fractures. Several factors can increase the risk of developing osteoporosis. Understanding these risks can help with early prevention and management. To estimate your own personal risk, use the FRAX® tool to assess fracture risk. The FRAX® tool has been developed to evaluate fracture risk of patients. It is based on individual patient models that integrate the risks associated with clinical risk factors as well as bone mineral density (BMD) at the femoral neck. Click here to access the tool.
1. Age & Gender
Bone density naturally decreases with age, particularly after 50.
Women are at higher risk, especially after menopause due to a drop in oestrogen levels.
2. Genetic & Family History
A family history of osteoporosis or fractures may increase the likelihood of developing the condition.
Certain ethnic backgrounds, such as Caucasian and Asian populations, have a higher predisposition.
3. Hormonal Imbalances
Low oestrogen (Women): Early menopause, hysterectomy, or conditions like PCOS can reduce oestrogen levels, affecting bone density.
Low Testosterone (Men): Decreased testosterone can contribute to bone loss.
Thyroid Disorders: Overactive thyroid (hyperthyroidism) or excessive thyroid hormone replacement therapy can weaken bones.
Parathyroid & Adrenal Gland Disorders: These conditions can interfere with bone metabolism.
4. Lifestyle & Dietary Factors
Poor Nutrition: A diet low in calcium, vitamin D, and protein can compromise bone strength.
Sedentary Lifestyle: Lack of weight-bearing and resistance exercises weakens bones over time.
Excessive Alcohol Consumption: Can interfere with bone formation and increase fall risk.
Smoking: Affects bone regeneration and reduces calcium absorption.
5. Medical Conditions That Affect Bone Health
Chronic conditions such as rheumatoid arthritis, kidney disease, liver disease, and diabetes can lead to bone loss.
Gastrointestinal disorders (e.g., coeliac disease, Crohn’s disease) can impair nutrient absorption, affecting bone strength.
6. Medications That May Increase Risk
Corticosteroids (e.g., Prednisone): Long-term use can lead to bone loss.
Anti-Seizure Medications: Some epilepsy treatments can affect bone metabolism.
Proton Pump Inhibitors (PPIs): Long-term use for acid reflux may reduce calcium absorption.
Cancer Treatments: Hormone therapies for breast and prostate cancer can contribute to bone thinning.
Preventing Osteoporosis
While some risk factors are unavoidable, lifestyle changes can significantly improve bone health. A balanced diet rich in calcium and vitamin D (Magnesium and Vitamin K are also helpful), regular weight-bearing exercises, and avoiding smoking and excessive alcohol can help maintain strong bones.
How Osteopaths Can Help Manage Osteoporosis
Osteopaths play a valuable role in supporting patients with osteoporosis by focusing on pain relief, mobility, and overall musculoskeletal health.
1. Pain Management
Gentle manual therapy techniques, such as soft tissue work and joint mobilization, can help reduce muscle tension and improve comfort, especially in areas affected by fractures or postural strain.
Addressing secondary musculoskeletal pain, such as compensatory tension in the back or hips, can improve overall well-being.
2. Improving Posture & Mobility
Osteopaths assess posture and biomechanics to help reduce stress on weakened bones.
Advice on optimal movement patterns can help prevent strain and improve balance, reducing the risk of falls.
3. Fall Prevention & Balance Training
Osteopaths can recommend exercises to improve coordination, balance, and proprioception, which are crucial in preventing falls and fractures.
Strengthening stabilizing muscles can enhance mobility and confidence in daily activities.
4. Exercise Prescription for Bone Health
Weight-bearing and resistance exercises help stimulate bone density and slow progression.
Tailored exercise programs focus on maintaining strength without excessive strain on fragile bones.
5. Lifestyle & Nutritional Advice
Guidance on maintaining a diet rich in calcium, vitamin D, and protein to support bone health.
Advice on lifestyle modifications, including quitting smoking, reducing alcohol intake, and maintaining an active lifestyle.
6. Collaborative Care
Osteopaths can work alongside GPs, physiotherapists, and other healthcare professionals to ensure comprehensive management.
Referral for further investigations, such as bone density scans, if osteoporosis is suspected but not yet diagnosed.
7. Emerging treatments
EMTT® Has shown some early promise in helping reduce low back pain associated with osteoporosis. EMTT® plays a significant role in bone fracture healing by enhancing various phases of osteoblastogenesis, which is the process of bone formation by osteoblasts. EMTT® is available at this clinic.
8. Who should have a DXA scan?
Women age > 65 yrs
Men age > 75 yrs
Younger patients with clinical risk factors
If you are concerned, we highly recommend speaking to your GP regarding scheduling a DXA scan. Should you prefer, affordable DXA scans are available privately. Body View offer both DXA and full body composition scanning, and we highly rate them.
For this cost-effective scanning service, I recommend booking with Body View, at Solent Business Park, Whiteley, Hampshire on 0330 043 7001. Existing MSO patients can get a 10% discount off the cost of their scans. Please get in contact with me for the online code.
For further information and guidance, why not join the Royal Osteoporosis Society? Lots of helpful information, and only £24/year (as of 2025).